Guests In Order of Appearance
-

Nigel Edwards
-

Sir Muir Gray
-

Gwyn Bevan
-

Anna Dixon MBE
-

Connie Jennings
-
Sir David Haslam
-

Angela Coulter
-

Neil Modha
Nigel Edwards
Nigel Edwards is an independent health policy expert working as an advisor with WHO and a number of UK organisations including PPL, NAPC, and HSMC Birmingham, where he is an honorary visiting professor.
Nigel was Chief Executive at the Nuffield Trust from 2012 to 2023. He has a long career in health policy and working on innovation and change in healthcare delivery and in providing challenging analysis on health policy. He has a strong interest in using different disciplines to inform health policy across a range of issues from new models of service delivery, primary care, local health strategy, and on wider health care policy in the UK and internationally.
Nigel’s current work in the UK has a focus on health policy, neighbourhood health, rural care, and strategy for small hospitals. For WHO he is helping to develop the rural primary care system in the Republic of Georgia and hospital strategy in North Macedonia. He is also developing policy briefings on urgent and emergency care and hospital strategy for WHO’s European Observatory on Health Systems and Policies.
Sir Muir Gray
Sir Muir Gray entered the Public Health Service by joining the City of Oxford Health Department in 1972 after qualifying in medicine in Glasgow, the city of his birth. The first phase of his professional career focused on disease prevention; for example, on helping people stop smoking. Then, using systems theory, he developed all the screening programmes in the NHS, for pregnant women, children, adults, and older people. He was awarded a CBE in 2005 for the development of the foetal, maternal, and child screening programme and the creation of the National Library for Health.
Muir started work in the NHS on Value-based Healthcare, arising from the work on Evidence-based Healthcare, and in 2001 published the first edition of How to Get Better Value Healthcare, a handbook in which was the first discussion about allocative value and the need for population-based healthcare. He published the first Annual Population Value Review for the Department of Health in 2004 and the first NHS Atlas of Variation, modelled on the Dartmouth Atlas of Healthcare, in 2010 and led the Rightcare programme promoting value-based healthcare.
Muir is now a director of the Oxford Value and Stewardship Programme and has published a series of How To Handbooks; for example, How to Get Better Value Healthcare first published in 2007, How to Build Healthcare Systems, How to Create the Right Healthcare Culture and, with Maggie Rae, Population Health Management, and How to Design and Develop Population Healthcare. There are also linked online learning programmes at Oxford Value and Stewardship.
Gwyn Bevan
Gwyn Bevan is emeritus professor of policy analysis in, and a former head of, the Department of Management at the London School of Economics and Political Science. He is an affiliate professor at L’Istituto di Management of the Scuola Superiore Sant’Anna, Pisa.
He has served on advisory committees to the Inspectorate of Police and Fire Services in England and Wales, the Education Commission of the Rockefeller Foundation on research in developing countries; and on government committees in England on allocating resources for healthcare and public health, the reform of publicly financed legal services, and funding research into overseas aid. He was director of the Office for Healthcare Performance at the Commission for Health Improvement (2001 to 2004), which was responsible for inspections of quality of care in the NHS in England and Wales.
In 2023 he published the highly acclaimed book How Did Britain Come to This? A century of systemic failures of governance.
Anna Dixon MBE
Anna Dixon is the Labour Member of Parliament for Shipley constituency in West Yorkshire. She is a member of the Public Accounts Committee, Co-Chair of the APPG Carers and APPG Housing and Care for Older People. Anna is a member of Community Trade Union, Labour Women’s Network, Christians on the Left, and the Fabian Society.
Prior to being elected Anna worked in a range of senior leadership roles in the health and social care sectors. She has nearly 30 years of experience in health and social care, with expertise in ageing and public health. She held a number of senior positions including Director of Strategy and Chief Analyst at the Department of Health and Social Care and Director of Policy at the King’s Fund. She also worked internationally for the World Health Organisation and the European Observatory on Health Systems and Policies.
A former Chief Executive of the Centre for Ageing Better and trustee on several boards, Anna led the development and delivery of both organisational and national strategies. She received an MBE for services to wellbeing in later life in the 2021 New Year’s Honours List. Anna chaired the Archbishops’ Commission on Reimagining Care (June 2021-Jan 2023) and served as a member of the Advisory Group to the Independent Review of Adult Social Care in Scotland (Sept 2020-Jan 2021). She is a trustee and Chair of Helpforce, a charity which supports volunteering in health and care.
Connie Jennings
Connie Jennings serves as the Director of Stronger Communities at Walsall Housing Group (whg) where she leads a team of passionate and dedicated professionals who work with people who face disadvantage and exclusion in their day-to-day lives. The majority of her team are whg customers who share their insights and lived experience with other customers and the wider community. Connie has over 25 years of experience in community development, regeneration, community engagement, and health equity.
Her mission is to address the root causes of inequality and improve the quality of life for whg customers and communities. She has successfully designed and delivered innovative projects and partnerships that increase social justice by reducing health inequalities, reducing poverty, improving skills, and increasing access to good work and careers. Some of the examples include the whg Community Champions programme which has lived experience as its fundamental building block, the H Factor Social Prescribing programme, the A.C.E Asthma programme designed to increase access to services and encourage self-care, and the Work4 programme helping whg customers gain good jobs in health, housing, and other sectors.
Sir David Haslam
Sir David Haslam is a writer and healthcare policy consultant, and past Chair of the National Institute for Health and Care Excellence (NICE). He is also past President and past Chairman of Council of the Royal College of General Practitioners, past President of the British Medical Association, and Professor of General Practice at the University of Nicosia, Cyprus. He was a GP in Ramsey, Cambridgeshire, for over 35 years, and is currently the chair of the charity “Young Lives vs Cancer”, a Non-Executive Director on Dorset Healthcare University NHS Trust, and an Associate with Kaleidoscope Health and Care.
David was named by Debretts and the Sunday Times as one of the 500 most influential and inspirational people in the United Kingdom. He was awarded CBE in 2004 for services to Medicine and Health Care and knighted in 2018 for services to NHS Leadership. His latest book – “Side Effects: How Our Healthcare Lost Its Way – And How We Fix It” – was published in August 2022 and was made Book of the Week in the Observer and listed in Waterstone’s Best Books of 2022.
Angela Coulter, PhD, Hon FRCGP, Hon FFPH
Angela Coulter is a retired academic with special interests in patient and public involvement and uses of personal health data. A social scientist by training, she has higher degrees in health services research from the University of London and the University of Oxford and is an associate fellow of Green Templeton College at the University of Oxford. She chairs Picker Institute Europe’s board of trustees, is a member of DARE UK’s programme board, and was the founding chair of HDR UK’s Public Advisory Board. Her previous roles included chief executive of Picker Institute Europe, director of policy and development at the King’s Fund, director of the Health Services Research Unit at the University of Oxford, director of global initiatives at the Informed Medical Decisions Foundation, and honorary professor at the University of Southern Denmark.
She has published more than 350 research papers, chapters, articles and reports and several books, including The Autonomous Patient, The European Patient of the Future, The Global Challenge of Healthcare Rationing, Hospital Referrals, Engaging Patients in Healthcare, Understanding and Using Health Experiences, A Stream of Lives, and her most recent book, Probing Deaths, Saving Lives, the story of a Victorian coroner and his inquests. She was the founding editor of Health Expectations, an international peer-reviewed journal on patient and public involvement in health care and health policy.
Neil Modha
Neil Modha is a GP with a keen interest in finding new efficient ways of working to help front line teams deliver the highest quality of care. He has extensive experience leading a large team of staff as an Accountable Officer in the Cambridgeshire and Peterborough Clinical Commissioning Group through authorisation into the first 4 years, and currently leads a GP federation (GPN) representing 270,000 patients. Neil also leads the Thistlemoor Medical Centre, a GP practice which is a training practice serving a population of 30,000 people amongst the most deprived in England. 80 percent of consultations take place in a language other than English.
Neil is co-chair of the local place-based board and an outpatient and diagnostics board. He recently led a work stream on data, population health management, and health inequalities in the Fuller Stocktake which featured in the Fuller review. In 2023 he was appointed as a Deputy Lieutenant of the King for Cambridgeshire and Peterborough.
In Memoriam Guests
We honour Jack Wennberg and John Stoeckle for their contributions to the study of practice variation and person-centred care. Their legacies underpin the argument for raising decision quality at the frontlines of care. They respected the contributions of earlier pioneers in their fields and did what they could to attract colleagues to the challenge of aligning policy with the frontline practices needed to give people the care they need and want, making health care sustainable for future generations.
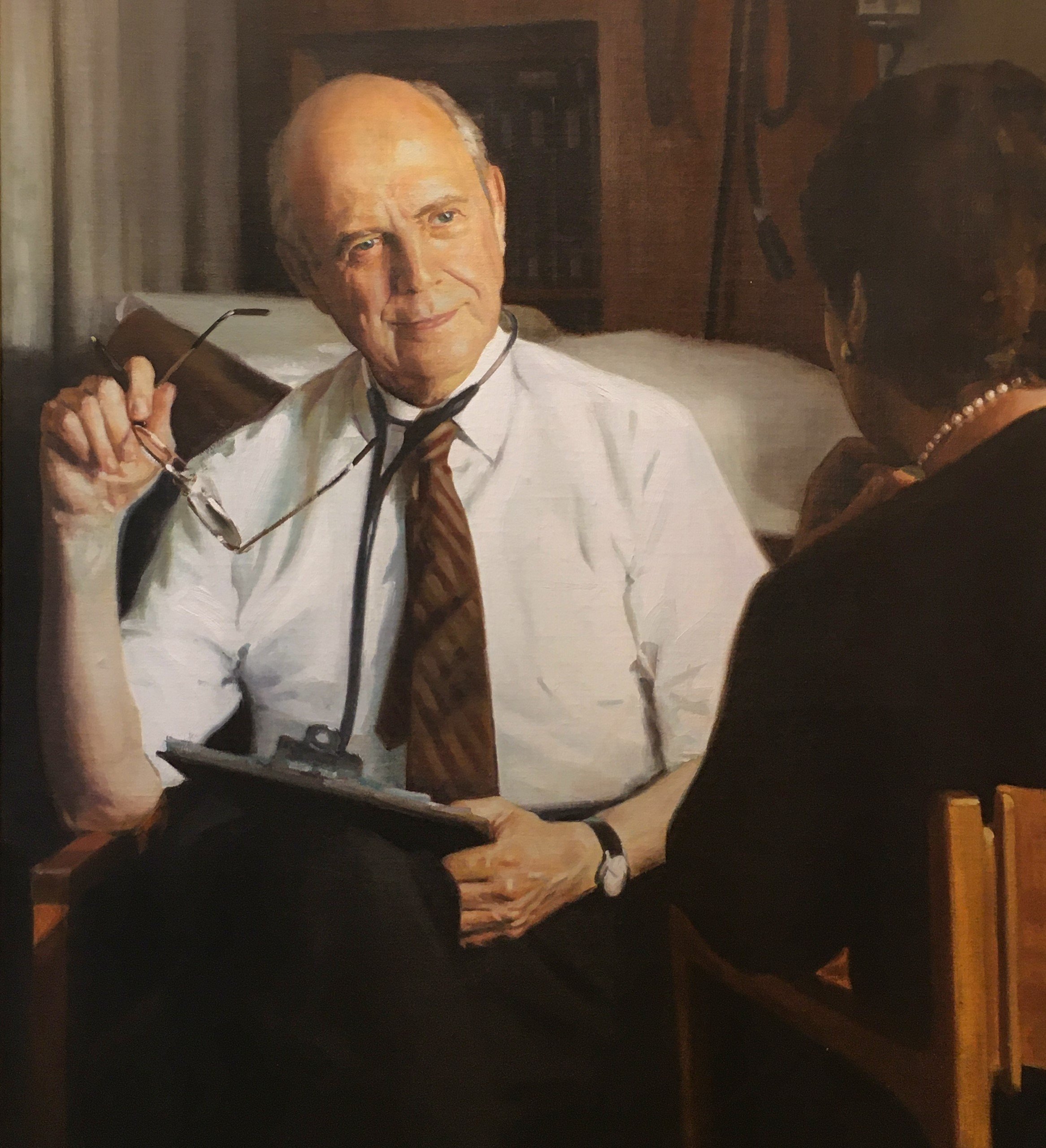
John D. Stoeckle, MD (1923 – 2020)
As a medical student at Harvard, John contracted tuberculosis and was sent to a sanatorium to recover with other medical students who had the same misfortune. It was a formative experience. John observed and learned from the doctors and nurses who cared for him, and equally from being a patient together with students, some of whom would not survive. John went on to a career marked by compassion and curiosity about what he called ‘patienthood’ as seen from the perspective of the patient and the doctor.
John personified patient-centred care with a deep appreciation for the emotional and social determinants of health. He inspired the development of community health centres and new programs to train clinicians who understood the importance of integrating primary with acute care, mental health with physical health, and medical care with social care. At the time of his death, he was remembered by those who knew him best as having a “healing presence like no other”.
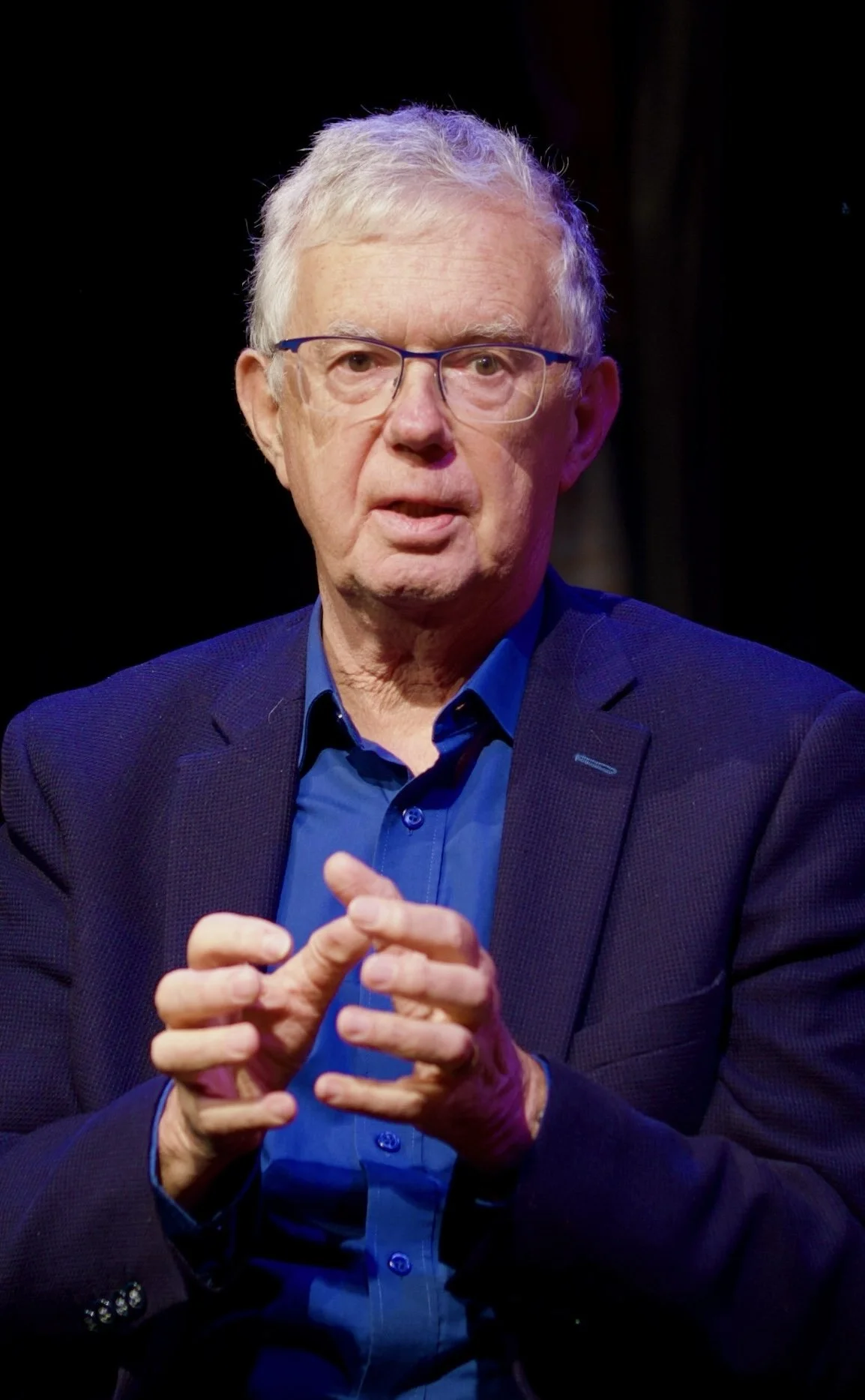
John E. (Jack) Wennberg, MD, MPH
(1934 – 2024)
Jack had a powerful intellect and a passion for doing the right thing. He used both traits to confront the powers that be in health care. No one understood better the resistance that constructive responses to practice variation would face. But Jack recruited researchers, clinicians, policy makers, and entrepreneurs who shared his values and joined the struggle. At the 2024 Wennberg International Collaborative Conference in Oslo, more than 100 colleagues from 17 countries honoured Jack for the gift he gave of a common vocation… to learn from variation to deliver what patients value most.